Knee replacement surgery has advanced significantly over the years, with innovations in implant design aimed at improving patient mobility and long-term outcomes. However, when it comes to single-radius (SR) vs. multi-radius (MR) femoral implants, how much of an impact does design really have on patient recovery and healthcare utilization? While clinical trials provide controlled comparisons, real-world evidence offers a broader perspective on outcomes across diverse patient populations.
To better assess these differences, OMNY Health analyzed real-world data from its orthopedic-focused medtech dataset, evaluating clinical, functional, and economic outcomes in TKA patients.
Comparing Implant Design in Real-World Settings
This study leveraged data from the OMNY Health Medical Device Database (2017-2021), examining 1,464 patients who underwent unilateral TKA. Patients were categorized into SR (N=1,135) and MR (N=329) cohorts, allowing for direct comparisons of key outcomes.
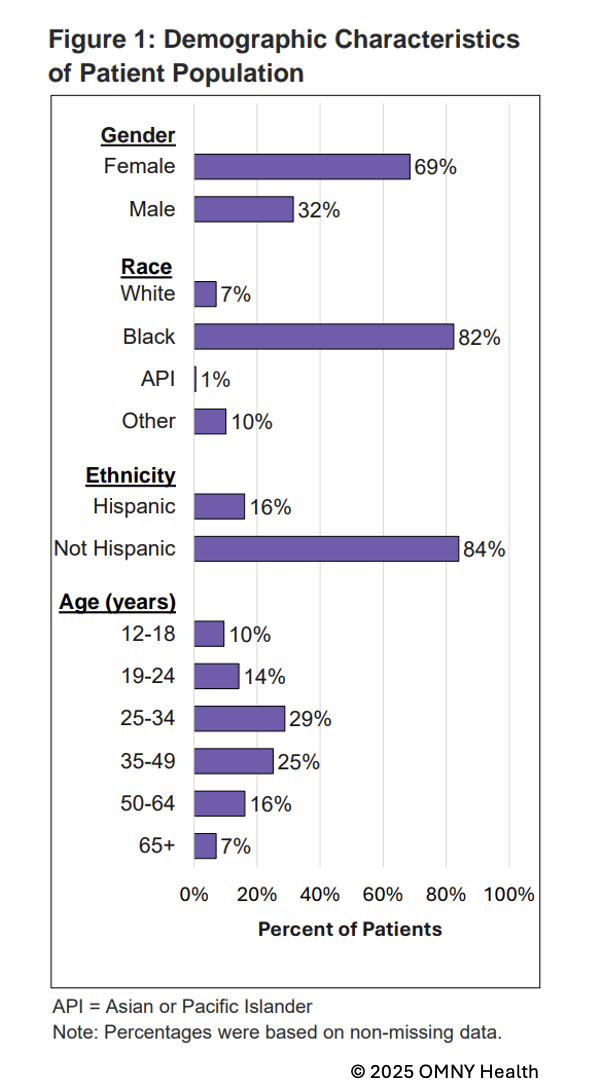
Patient Demographics:
- Most patients were born between the 1950s and 1960s (SR: 59%, MR: 57%).
- Women accounted for the majority of cases (SR: 63%, MR: 70%).
- The SR cohort had a higher proportion of White patients (85%) compared to the MR cohort (75%).
- More MR patients underwent outpatient procedures (53%) compared to SR patients (43%).
Key Findings: Minimal Differences Between Implant Designs
Despite prior speculation that implant design could significantly impact outcomes, this real-world analysis found that SR and MR implants performed similarly across key measures.
Clinical Outcomes:
- Mortality rates were low in both cohorts (SR: 1.1%, MR: 0.3%).
- Postoperative knee pain was reported at comparable rates (SR: 0.6%, MR: 1.2%).
- Implant removal was rare, with no significant difference observed (SR: 0.4%, MR: 0.0%).
Functional Outcomes:
- Non-routine discharge disposition (NRDD) rates were identical (SR: 16.4%, MR: 16.4%), suggesting that implant design did not influence post-surgical mobility.
Economic & Utilization Outcomes:
- Length of stay (LOS) was similar across groups (SR: 0.98 days, MR: 0.96 days).
- Gross charges were slightly higher for SR patients (Median: $43,879 vs. $39,255 for MR), though differences may be driven by factors beyond implant design.
What This Means for Clinical Decision-Making
The findings suggest that implant design alone does not significantly impact clinical or functional outcomes in TKA patients. Instead, factors such as surgical technique, rehabilitation protocols, and patient-specific factors play a more substantial role in determining recovery and long-term success.
For healthcare providers and medtech companies, these results highlight the value of real-world data in refining orthopedic product development and post-market surveillance. While MR designs have been thought to provide more natural knee movement, this study suggests that real-world functional outcomes do not differ significantly between SR and MR implants.
Additionally, the slight difference in cost between implant types warrants further investigation to determine cost-effectiveness in value-based care models.
The Role of Real-World Data in Orthopedic Research
By integrating structured EHR data with curated clinical measures, OMNY Health provides real-world insights into medical device performance. This data-driven approach enables:
- Comparisons of implant designs and surgical techniques to refine best practices.
- Better understanding of patient recovery patterns and healthcare utilization.
- Support for evidence-based decision-making to optimize orthopedic device selection and patient outcomes.
With orthopedics as a key therapeutic area for medtech innovation, leveraging real-world evidence is essential for ensuring high-quality, cost-effective decision-making in TKA and beyond.