Breaking Barriers in Sickle Cell Care: Real-World Insights on Treatment & Healthcare Utilization
Sickle cell disease (SCD) presents unique challenges for patients and healthcare providers alike. To better understand these challenges, OMNY Health analyzed real-world data (2017-2024), leveraging its unique ability to integrate structured EHR data with curated clinical measures to provide a comprehensive view of SCD patients. This study examined the demographics, healthcare utilization, and treatment patterns of 10,958 individuals diagnosed with SCD.
Disproportionate Burden and Frequency of Healthcare Use in Sickle Cell Disease
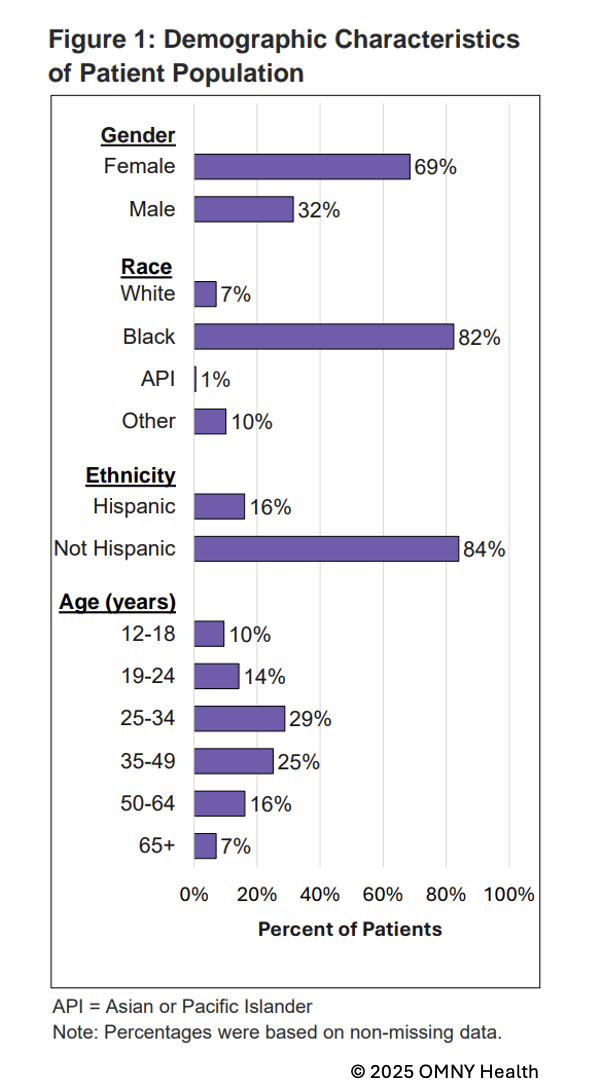
SCD remains a condition that disproportionately affects minority populations. Among the studied population:
- 82% identified as Black, with additional representation from Hispanic and Asian/Pacific Islander groups, emphasizing racial disparities in disease burden and healthcare access.
- The average age of patients was 37 years, showing that SCD continues to impact individuals well into adulthood.
Figure 1. Demographic Characteristics of Patient Population
- 66% had an emergency room visit.
- 65% required outpatient care.
- 4.3 inpatient admissions per patient on average, though some required over 185 hospital stays.
Comorbidities and Limited Treatment Utilization for Sickle Cell Disease
OMNY Health’s curated datasets capture a wide range of comorbidities, helping to broader clinical patterns that impact SCD progression. Among the most common conditions observed:
- Anemia, chronic pain, and hypertension, which are linked to SCD progression.
- Gastroesophageal reflux disease (GERD), urinary tract infections, and vitamin D deficiency, highlighting broader health vulnerabilities.
These figures suggest that many individuals with SCD struggle with disease management, pain crises, and complications that lead to recurring hospital visits. The high frequency of inpatient admissions, even among younger adults, indicates that preventive strategies may not be reaching those who need them most. Many hospital stays are driven by acute complications, highlighting the importance of early intervention and better access to disease-modifying treatments that could reduce the need for emergency care.
Table 1: HCRU Among Individuals with SCD
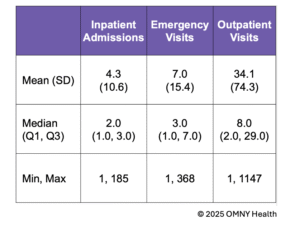
Figure 2: Top clinical comorbidities among individuals with SCD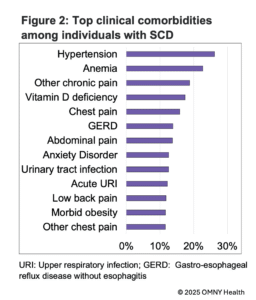
Despite available treatments, adoption remains low:
- 11.3% of eligible patients received hydroxyurea, the most used therapy.
- Less than 1.1% of patients received newer disease-modifying treatments, such as Crizanlizumab, Voxelotor, L-glutamine, or Stem Cell transplants.
This raises concerns about barriers to access, including cost, provider awareness, and prescribing patterns. Through OMNY Health’s ability to track real-world prescribing trends and treatment adherence, stakeholders can better understand where interventions are needed to improve access.
Moving Forward with Data-Driven Solutions
By leveraging OMNY Health’s robust real-world data, we can provide critical insights into treatment patterns, healthcare utilization, and patient needs. OMNY Health’s curated data and clinical measures enable a more complete understanding of SCD care gaps, supporting efforts to inform policy changes, optimize treatment strategies, and enhance healthcare provider decision-making
For more information about OMNY Health’s product offerings, let’s connect!
